This post is also available in:
![]() 简体中文 (Chinese (Simplified))
简体中文 (Chinese (Simplified)) ![]() ไทย (Thai)
ไทย (Thai) ![]() 한국어 (Korean)
한국어 (Korean)
Trichomoniasis (commonly known as ‘trike’ or ‘trich’) is a sexually transmitted infection (STI) caused by a parasite. It can cause inflammation and infection of the urethra, vagina, and cervix and can infect people of all genders. It usually transmits during sexual contact but can also be transmitted by sharing wet towels or washers.
Around 70% of people with trichomoniasis do not experience symptoms. If you do get symptoms, they can include a smelly, yellow-green vaginal discharge with irritation of the vulva. You can spread the infection even if you don’t have symptoms. Trichomoniasis is treatable with antibiotics.
Signs and Symptoms
If symptoms appear, it will usually be within 5 to 28 days of exposure. If left untreated, trichomoniasis is associated with infertility, pelvic inflammatory disease and enhanced risk of HIV transmission. Having trichomoniasis causes irritation in the genital area, making it easier for other STI to enter the body or be transmitted to others.
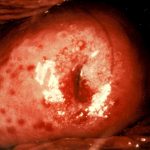
Vagina/Vulva
Trichomoniasis can show no symptoms. If you do get signs or symptoms, there may be:
- Frothy or smelly vaginal discharge that is yellow, grey or green
- Vaginal itching or burning
- Pain low in the tummy
- Pain during sex or when urinating
Penis
Trichomoniasis is often asymptomatic in people with penises. If signs or symptoms are present, there may be:
- Burning or pain when passing urine
- Discharge from the opening of the penis
Transmission
Trichomoniasis is primarily transmitted through unprotected/”natural” vaginal sex. It can also spread through:
- vaginal discharge on hands or sex toys
- direct vulva to vulva contact
- sharing wet towels or washers
Trichomoniasis cannot be transmitted to the mouth and anus.
You can still pass on trichomoniasis when you don’t have symptoms.
Prevention
The best way to prevent getting trichomoniasis is to use condoms during vaginal sex and change condoms between partners when using toys or doing doubles/group bookings.
It is recommended that you always change condoms when going from anal to vaginal or oral sex.
Testing
Here’s some information about testing for trichomoniasis. You can view a list of sex worker-friendly sexual health clinics on our Where To Test page.
Testing Method
- Urine sample (all genders)
- Vaginal swabs for people with vaginas
When to Test
- It is possible to get a positive test within a week of exposure, but some infections may not show for a month. You may need to test more than once if you are concerned you may have trichomoniasis.
- Test if you have a sexual partner who has been diagnosed with the infection.
Other Info
- Trichomoniasis is not included in routine STI testing, so you may need to request a test from your doctor or nurse.
- Sexual health clinic testing is often bulk billed, even if you don’t have Medicare, so the test will most likely be free.
- You may pay a fee or be bulk billed if you see a GP.
Treatment
Trichomoniasis is treatable with antibiotics. Here’s what you need to know about treating it.
Treatment Method/s
- Usually, a single-dose antibiotic.
Costs and Other Information
- To prevent reinfection, treat partners at the same time, even if they don’t have symptoms.
- Treatment costs will depend on which antibiotic you are prescribed.
- Sexual health clinic treatments are often bulk billed, even if you don’t have Medicare, so the treatment may be free.
- You may pay a fee or be bulk billed if you see a GP.
- Trichomoniasis is cured by effective treatment, but you do not develop immunity. It is possible to get trichomoniasis again.
How might this impact my work?
Practical Considerations
- It is recommended that you do not have sex for 7 days after treatment.
- If you can’t avoid having sex, then using a condom will help lower the chance of transmitting trichomoniasis, but there is no guarantee.
- Some antibiotics can reduce the effectiveness of oral contraception (‘the pill’).
- If you often get thrush when you take antibiotics, you may want to take probiotics during and after your treatment to help prevent this.
- You should inform any recent doubles partners if you test positive for trichomoniasis.
Legal and Reporting Considerations
- Some states and territories may have laws that criminalise sex working or having sexual contact while you have a BBV or STI. Check out our BBV, STI and the Law resource or contact your local sex worker peer organisation for more information.
- Contact tracing of previous sexual partners (also known as ‘partner notification’) is a consideration for some BBV and STI. It should be done with consideration of the unique transmission risk and privacy needs of sex workers. Your local sex worker peer organisation can advise on any partner notification process to ensure that it is appropriate for your circumstances.